Unraveling the Distinctions: Type 1 vs. Type 2 Diabetes
Diabetes is a chronic condition that affects millions of people worldwide. It is characterized by high blood sugar levels due to the body’s inability to produce or effectively use insulin, the hormone responsible for regulating glucose levels. While there are different types of diabetes, the two most common forms are Type 1 and Type 2 diabetes. Although they share some similarities, understanding their key differences is crucial for effective management and treatment. In this article, we will delve into the dissimilarities between Type 1 and Type 2 diabetes and shed light on their distinctive characteristics.
Type 1 Diabetes: The Autoimmune Condition
Type 1 diabetes, previously known as juvenile diabetes or insulin-dependent diabetes, is an autoimmune disease. In this form of diabetes, the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. As a result, the body is unable to produce insulin, leading to high blood sugar levels.
Causes and Risk Factors
The exact causes of Type 1 diabetes are still not fully understood. However, genetic predisposition and certain environmental factors, such as viral infections, may contribute to its development. It typically appears during childhood or adolescence but can occur at any age.
Symptoms
Symptoms of Type 1 diabetes usually develop rapidly and can include excessive thirst, frequent urination, unexplained weight loss, extreme hunger, fatigue, and blurred vision.
Treatment
People with Type 1 diabetes require insulin therapy to survive. Insulin is administered through injections or an insulin pump to replace the insulin their body cannot produce. Additionally, careful monitoring of blood sugar levels, a balanced diet, regular exercise, and continuous education on self-management are vital aspects of treatment.
Type 2 Diabetes: The Lifestyle-Related Condition
Type 2 diabetes, previously referred to as adult-onset diabetes or non-insulin-dependent diabetes, is the most common form of diabetes, accounting for the majority of cases. Unlike Type 1 diabetes, Type 2 diabetes is primarily characterized by insulin resistance, meaning the body’s cells do not respond effectively to insulin.
Causes and Risk Factors
Type 2 diabetes is strongly linked to lifestyle factors, such as poor diet, sedentary lifestyle, obesity, and a family history of the condition. While genetic factors play a role, lifestyle choices greatly influence its development. It is more common in adults, but the rising prevalence of childhood obesity has led to an increase in Type 2 diabetes cases among young individuals.
Symptoms
Symptoms of Type 2 diabetes may develop gradually and can include increased thirst, frequent urination, fatigue, blurred vision, slow wound healing, and recurring infections.
Treatment
Treatment for Type 2 diabetes often begins with lifestyle modifications, including a healthy diet, regular exercise, weight management, and smoking cessation if applicable. In some cases, oral medications or injectable therapies may be prescribed to help manage blood sugar levels. In more advanced cases, insulin therapy may be necessary.
Key Differences Between Type 1 and Type 2 Diabetes
Cause
Type 1 diabetes is an autoimmune disease, while Type 2 diabetes is primarily caused by lifestyle factors, although genetics can contribute.
Age of Onset
Type 1 diabetes typically appears during childhood or adolescence, whereas Type 2 diabetes is more common in adults, although it is increasingly affecting younger individuals.
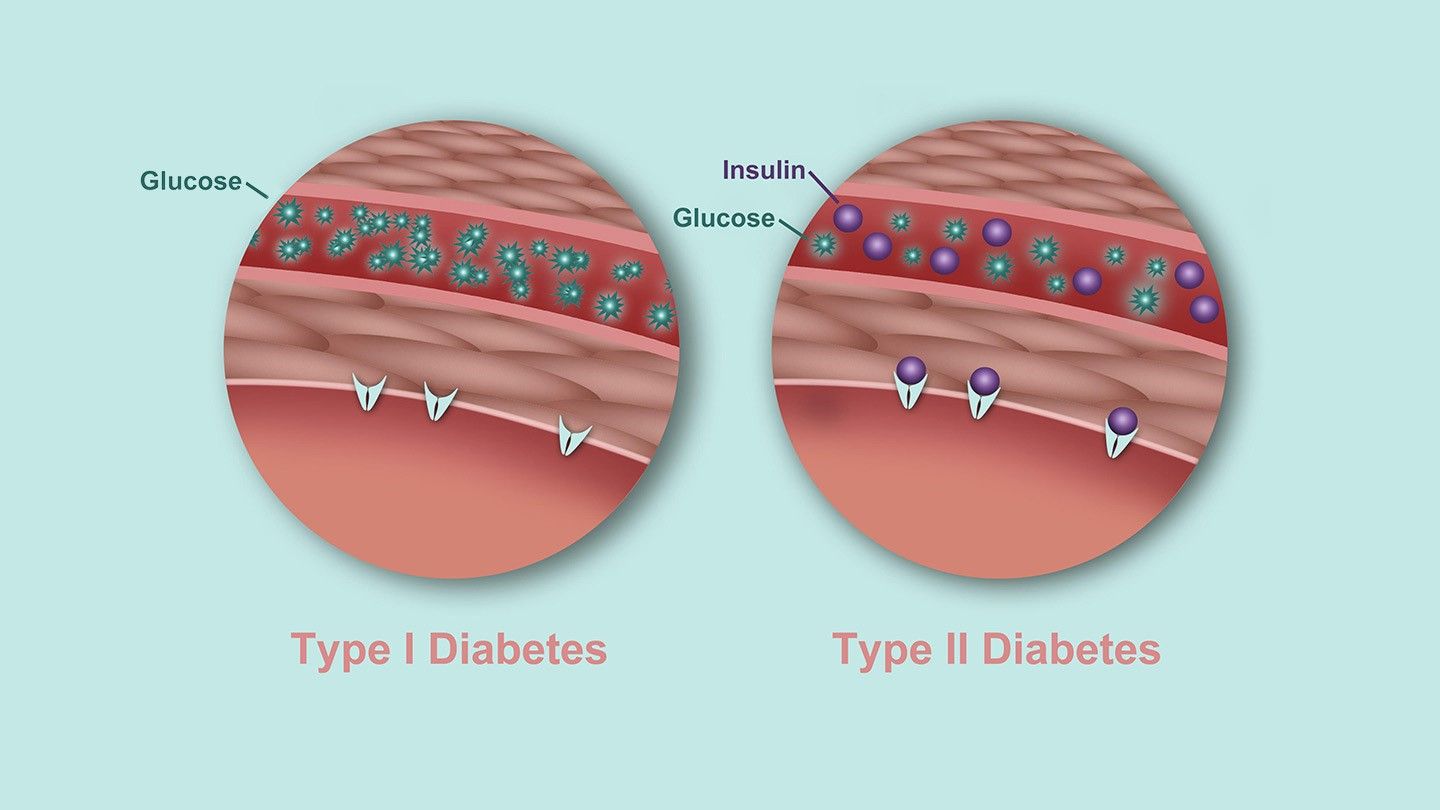
Insulin Production
In Type 1 diabetes, the body does not produce insulin, whereas in Type 2 diabetes, the body either does not produce enough insulin or cannot use it effectively (insulin resistance).
Treatment Approach
People with Type 1 diabetes require insulin therapy for survival. In Type 2 diabetes, treatment may involve lifestyle modifications, oral medications, injectable therapies, or insulin therapy, dependingon the severity and progression of the condition.
Risk Factors
Type 1 diabetes is often associated with genetic predisposition and autoimmune factors. Type 2 diabetes is strongly linked to lifestyle factors such as poor diet, sedentary lifestyle, obesity, and family history, although genetics also play a role.
Progression
Type 1 diabetes usually progresses rapidly, whereas Type 2 diabetes may develop slowly over time.
While both Type 1 and Type 2 diabetes share the common characteristic of elevated blood sugar levels, they have distinct differences in terms of cause, age of onset, insulin production, treatment approaches, and risk factors. Type 1 diabetes is an autoimmune condition that requires insulin therapy for survival, while Type 2 diabetes is primarily influenced by lifestyle factors and may be managed through lifestyle modifications, medications, or insulin therapy. Understanding these differences is crucial for individuals affected by diabetes, healthcare professionals, and the general public to promote effective management, early detection, and prevention strategies.